BEST SELLERS
-
Dermlite DL5
Regular price $1,895.00Regular priceUnit price per -
DermLite DL200 Hybrid
Regular price $1,050.00Regular priceUnit price per -
DermLite DL100
Regular price $395.00Regular priceUnit price per -
DermLite DL4
Regular price $1,695.00Regular priceUnit price per -
MagnetiConnect® Clamp (MCC)
Regular price $90.00Regular priceUnit price per -
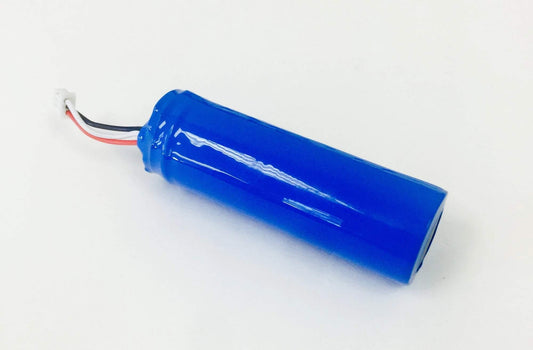
Battery for DL4/DL4W
Regular price $59.00Regular priceUnit price per
FAQs
Who should I contact if I have question?
The best way to reach us is by email 'contact@dermatoscopes.com' or use our online contact form.
How can I cancel or change my order?
Orders may be cancelled (or changed) at any point prior to shipping. To do so, please email us at 'contact@dermatoscopes.com.'
How can I return a product?
Purchases are subject to the following terms:
Physical Merchandise (see next section for "Gift Card" terms and conditions)
Broken or defective merchandise should be reported to us immediately upon receipt and returned for replacement or credit within 30 days of shipment.
Before returning any items, please first contact us (contact@dermatoscopes.com) to describe any such issues.
For all other returns, a full refund will be made for items returned within 30 days of shipment that are in resellable condition*. This includes providing the original packaging, instructions and any other contents of the product as it arrived upon initial purchase.
As stated above, please first contact us to arrange any return prior to shipping the item(s) back.
Proper packaging of returned items must be used to prevent damage during shipment. We also recommend that you insure the package. Shipping charges to return merchandise to dermatoscopes.com are the buyer's responsibility (except in the case of defective merchandise received).
With the above policy in mind, just know that we want you to be 100% satisfied with your purchase and we will do our best to accommodate any reasonable return requests.
However, due to the nature of what we sell (dermatoscopes and accessories) and our relationship with the manufacturer (we are a Dermlite distributor), we recognize that every situation is unique. So above all, please first contact us if you're ever concerned about your purchase and feel the need to either return/exchange your purchase.
contact@dermatoscopes.com
*We unfortunately need to place emphasis on the policy that full refunds are available for items in resellable condition. Signs of significant use (scratches, scuffs, etc.), missing items, damaged/missing boxes, etc. can affect your ability to receive a full refund.
Therefore, we respectfully ask that you please keep all of your"new box" items and handle your purchase with care until you absolutely know that you're happy with your purchase. Thank you!
Gift Cards
Dermatoscopes.com offers "virtual" gift cards (aka "e-gift cards). Recipients should treat their "virtual gift card" like cash (especially its unique gift code) as we cannot accept responsibility for unauthorized use. Gift cards are redeemable for purchases only at dermatoscopes.com. Except where required by state law, gift cards cannot be replaced if lost or stolen. Gift cards cannot be returned, refunded, or redeemed for cash. Purchases made using a gift card will be deducted from the card balance until its value reaches zero. Gift card recipients are asked to use their gift card in a timely manner, as any remaining balance (and the card itself) will be void after 5 years from initial date of purchase.
Repairs and Warranty Service
Repairs and service are performed by the Dermlite service center (a separate entity from dermatoscopes.com). A “Request for Repair” form is required to be completed prior to sending in your item for repair. Upon completing the above online form, Dermlite service and repair department will contact you with further details and instructions for completing the repair process.
How long will it take to get my package?
If your order is "urgent" and/or can only be received within a specific time frame, please contact us before placing your order.
We fulfill most orders within 1-2 business days (Mon-Fri). However, delays sometimes can (and do) occur. Please note that "tracking emails" are sent out automatically once we've fulfilled an order, so be sure to keep an eye on your email inbox.
Please also note that dermatoscope orders are typically shipped out via USPS and require an adult signature for delivery.
As a Dermlite distributor, we fulfill most orders ourselves. However, some Items are instead processed directly by Dermlite headquarters (in California). Those fulfillments may take a bit longer to be processed, but are typically shipped out within 3 business days.

Dermlite Dermatoscopes
From the "pocket-friendly" DL1 to the most advanced DL5, we'll help you find the dermatoscope which is right for you!

Photo Dermoscopy Devices
Whether simply adding photos to the patient medical records or building your own personal learning library, we can help you connect your dermatoscope to your favorite camera or smartphone!
.png?v=1667978305)